Understanding Coronary Artery Disease and Heart Attacks
A Scientific Deep Dive
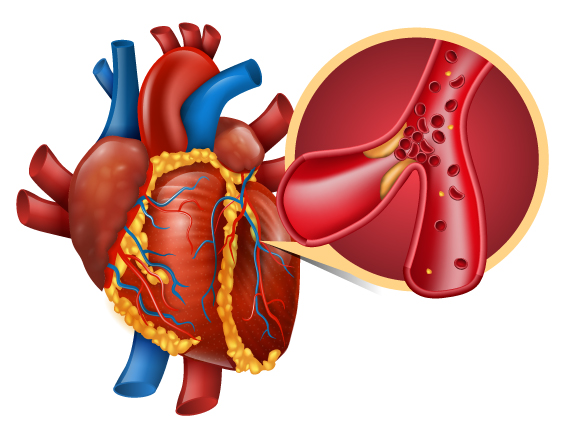
The human heart is often described poetically, but scientifically, it is a tireless muscular pump—the myocardium—that requires a constant supply of oxygen and fuel. When that supply line is cut, the result is a Myocardial Infarction (MI), commonly known as a heart attack.
This article breaks down the complex pathology of Coronary Artery Disease (CAD) and heart attacks into clear, scientific, yet accessible language.
1. The Root Cause: Coronary Artery Disease (CAD)
A heart attack is rarely a sudden, random event. It is usually the climax of a decades-long process called Atherosclerosis.
The “Fatty Streak” and Plaque Formation
It begins microscopically, often in childhood or early adulthood.
- Endothelial Injury: The inner lining of your arteries (the endothelium) is smooth like Teflon. Factors like high blood pressure, smoking, or high blood sugar cause micro-tears in this lining.
- Infiltration: “Bad” cholesterol (LDL) slips into these cracks and gets trapped in the artery wall.
- The Immune Response: Your body perceives this trapped cholesterol as an intruder. It sends white blood cells (macrophages) to eat the cholesterol. These cells become engorged with fat and turn into “Foam Cells.”
- Plaque Build-up: Over time, these foam cells accumulate, calcify, and are covered by a hard fibrous cap. This structure is called an atherosclerotic plaque.
The Danger: As the plaque grows, it narrows the artery (stenosis), restricting blood flow. This often causes Angina (chest pain during exertion), as the heart struggles to get enough oxygen through the narrowed pipe.
2. The Event: Anatomy of a Heart Attack
A heart attack typically occurs not because the plaque grows until it blocks the artery 100%, but because the plaque ruptures.
Explore
The Rupture and Clot
- Instability: Inflammatory chemicals can weaken the fibrous cap of the plaque. Suddenly, it tears open.
- The Clot (Thrombus): The material inside the plaque is highly “thrombogenic”—it triggers instant clotting. Platelets in your blood rush to the site to seal the tear, forming a clot.
- Occlusion: This clot forms so rapidly that it can completely block the artery.
- Ischemia: The heart muscle (myocardium) downstream from the blockage is instantly starved of oxygen.
The “Golden Hour” of Necrosis
Time is muscle. When oxygen is cut off, heart muscle cells don’t die instantly—they suffocate slowly.
- 0–20 Minutes: The cells stop contracting to save energy. This is “stunning.” Damage is still reversible.
- 20+ Minutes: Cells begin to die (necrosis). They burst open, leaking proteins like Troponin into the bloodstream. (This is why doctors check Troponin levels to diagnose a heart attack).
- 6–12 Hours: If blood flow isn’t restored, the damage becomes permanent scar tissue.
3. Classifying the Attack: STEMI vs. NSTEMI
Doctors classify heart attacks into two main scientific categories based on the ECG (Electrocardiogram) reading.
| Type | Full Name | What it Means |
| STEMI | ST-Elevation Myocardial Infarction | Total Blockage. The “classic” massive heart attack. The coronary artery is 100% blocked by the clot. The ECG shows a specific “ST-Elevation” pattern indicating full-thickness damage to the heart wall. |
| NSTEMI | Non-ST-Elevation Myocardial Infarction | Partial Blockage. The artery is severely narrowed or only partially blocked by the clot. Damage is occurring, but it may not penetrate the full thickness of the heart wall. |
4. Symptoms: Beyond the “Hollywood” Heart Attack
While chest crushing pain (often described as an “elephant sitting on the chest”) is common, biological variation means symptoms differ.
- Referred Pain: The brain often confuses pain signals from the heart with signals from the arm, jaw, neck, or back. This is why you might feel a heart attack in your left shoulder or teeth.
- Autonomic Symptoms: Nausea, cold sweats (diaphoresis), and lightheadedness occur because the heart attack activates the nervous system’s “fight or flight” response.
- Silent MI: In diabetics and the elderly, nerve damage or altered pain perception may lead to a “silent” heart attack with no chest pain at all—only shortness of breath or fatigue.
5. Modern Treatments: Reopening the Pipes
The goal of treatment is Reperfusion—restoring blood flow before the muscle dies.
- Angioplasty & Stenting (PCI): This is the gold standard. A catheter (a long, thin tube) is threaded through an artery in the wrist or groin up to the heart. A balloon at the tip is inflated to smash the plaque against the wall, and a wire mesh tube (stent) is left behind to keep the artery open.
- Thrombolytics: If a hospital doesn’t have a cath lab, “clot-busting” drugs are injected to dissolve the blood clot chemically.
- CABG (Bypass Surgery): If the blockages are too complex for stents, surgeons take a healthy vein from the leg or artery from the chest and sew it onto the heart to “bypass” the blocked section.
Summary Checklist for Heart Health
- Understand your lipids: High LDL creates the plaque; High HDL helps remove it.
- Control blood pressure: Hypertension causes the initial injury to the artery wall.
- Recognize the signs: Time is the most critical factor in saving heart muscle.
Stay Informed – Stay Healthy