The Science of the Coronary Angiogram
Why the “Gold Standard” Test is Vital for Heart Health
If a heart attack is a “plumbing problem,” then a Coronary Angiogram is the ultimate blueprint. While stress tests and ECGs give doctors clues, an angiogram provides definitive, high-definition proof of exactly where and how severely your arteries are blocked.1
This article explores the technical precision, the “why,” and the “how” of this life-saving procedure.
1. The Purpose: Why Do We Need an Angiogram?
Doctors don’t order invasive procedures lightly. A coronary angiogram (often called “cardiac cath”) is the Gold Standard diagnostic tool for Coronary Artery Disease (CAD).2
Common Indications:
- Acute Coronary Syndrome (ACS): If you are having a heart attack (STEMI or NSTEMI), this test is urgent to locate the clot.
- Unstable Angina: Chest pain that is unpredictable or occurring at rest.3
- Positive Stress Test: If a treadmill or nuclear stress test suggests ischemia (lack of blood flow), an angiogram confirms the diagnosis.
- Pre-Surgical Clearance: Before major open-heart surgery (like valve replacement), surgeons need to ensure the coronary arteries are clear.
2. The Procedure: A Technical Walkthrough
The procedure is performed in a specialized sterile room called a Cardiac Catheterization Lab (Cath Lab).4 It is not open surgery; it is a percutaneous (through the skin) procedure.5
Step 1: Vascular Access (The Entry Point)
Using the Seldinger Technique (a needle-wire-catheter method), the doctor gains access to the arterial system.6
- Radial Access (Wrist): The modern preference. Accessing the radial artery in the wrist reduces bleeding risk and allows patients to sit up immediately after the procedure.7
- Femoral Access (Groin): The traditional route. Used if the wrist arteries are too small or tortuous.
Step 2: The Journey to the Heart
A catheter—a long, hollow, flexible tube about 2mm wide—is threaded over a guidewire.8
- It travels from the wrist/groin $\rightarrow$ Subclavian/Iliac artery $\rightarrow$ Aorta.
- Target: The catheter tip is carefully hooked into the Ostium (the opening) of the coronary arteries, located just above the aortic valve.
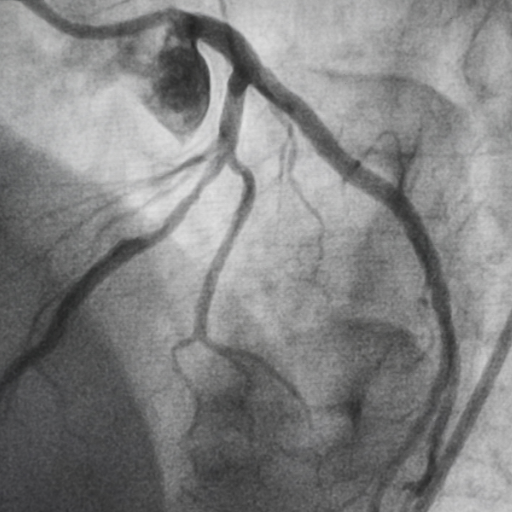
Step 3: Cine-Angiography (The “Movie”)
This is the critical moment.
- Contrast Injection: An iodine-based radio-opaque dye is injected through the catheter directly into the coronary artery.9
- Fluoroscopy: An X-ray camera (C-arm) rotates around the patient, filming at 15–30 frames per second.10
- Visualization: Since X-rays cannot see soft tissue, they track the dye.11 The dye fills the artery, creating a black “cast” of the vessel interior on the screen.12
What the Doctor Sees: A healthy artery looks like a smooth, wide river. A diseased artery looks like a “bitten apple core” (stenosis) or an abrupt cut-off (total occlusion/blockage).
3. The Patient Experience
- Conscious Sedation: You are usually awake but relaxed with sedatives (like Versed/Fentanyl).13 You are not under general anesthesia.14
- The “Hot Flush”: When the dye is injected, you may feel a sudden, brief wave of warmth spreading from your chest to your pelvis.15 This is a normal reaction to the contrast medium.16
- Ad-Hoc PCI: If a critical blockage is found during the diagnostic angiogram, the doctor may immediately switch to an interventional procedure to place a Stent (a metal scaffold) to open the artery.17
4. Risks and Safety Profile
While generally safe, it is an invasive procedure with specific biological risks:
| Risk Factor | Technical Explanation |
| Contrast Nephropathy | The iodine dye can be toxic to kidneys, especially in diabetics or those with pre-existing kidney disease. Hydration is key. |
| Vascular Injury | Rarely, the catheter can scrape or dissect the artery wall (dissection) or cause a bleed at the puncture site (hematoma). |
| Allergic Reaction | Mild hives or anaphylaxis to the iodine contrast agent. |
| Stroke/Embolism | extremely rare (<0.1%), but a piece of plaque could theoretically be dislodged by the catheter. |
5. Who Performs It and Where?
- The Specialist: An Interventional Cardiologist.18 This is a doctor with extra years of training specifically in catheter-based procedures, distinct from a general cardiologist.
- The Setting: A hospital with a dedicated Cath Lab and, ideally, surgical backup (cardiothoracic surgery team) in case of rare emergencies.19
Summary
A coronary angiogram is the bridge between suspecting a heart problem and fixing it.20 It transforms vague symptoms into a visual map, allowing doctors to decide between medication, stenting, or bypass surgery.21